There is a fine difference between health education and health literacy but it can make all the difference in the health of your patients and their ability to comply with treatment. One teaches patients about their health and ways to improve it while the other is the degree to which a patient can make appropriate health decisions. It’s all part of the continuum of health education that helps patients engage in their own health. Both are essential to improving outcomes.
Patient Education Can Reduce Costs
The extent to which patients are educated about their health conditions is considered one of the most important aspects of chronic disease management. It shares information with the patient and brings them along the care journey in a realistic and informed manner. It can improve compliance and in the best case scenarios, can reduce rehospitalizations.
Nowhere is education more important than in cases of complex diagnosis, life-altering or life-threatening diagnosis. Patient Engagement HIT recently reported Peter Goldbach, MD, Chief Medical Officer of Health Dialog as saying, “Sometimes what gets lost is the fact that the patient you’re working with may not really understand their condition. It’s very confusing to be a patient, (especially when) it takes the provider awhile to arrive at a diagnosis. But eventually providers need to share that diagnosis with the patient, let them understand it, and have a chance to let it sink in.”
Given the cancer rate alone in the US, patient education in cases of difficult diagnoses is essential. The American Cancer Society estimates that in 2018, there will be an estimated 1,735,350 new cancer cases diagnosed in the US and 609,640 cancer deaths.
Chronic disease is even more prevalent. HealthyPeople.gov of the Office of Disease Prevention and Health Promotion reports:
- Chronic diseases are the leading cause of death and disability in the United States, causing 7 out of 10 deaths each year.
- Heart disease, cancer, and stroke alone cause more than 50% of all deaths each year.
- In 2008, 107 million Americans—almost 1 out of every 2 adults age 18 or older—had at least 1 of 6 reported chronic illnesses:
- Cardiovascular disease
- Arthritis
- Diabetes
- Asthma
- Cancer
- Chronic obstructive pulmonary disease (COPD)
In addition, the US population is aging. As Baby Boomers reach age 65+ and chronic disease is expected to increase.
Leading experts on diabetes agree wholeheartedly that patient education is essential. A joint position statement by the American Diabetes Association, the American Association of Diabetes Educators and Academy of Nutrition and Dietetics said that it is important for healthcare providers and their practices “to ensure that patients with Type 2 diabetes receive both diabetes self-management education and support in a consistent manner”. It facilitates better self-management decisions in what is often complex self-care.
Effective Patient Education Methodologies
There are several patient education methodologies that healthcare professionals find effective. They include:
- Teach-back: In this method, the patient receives education on health issues and then repeats the information back to the “teacher”. One study found that this method of patient education can reduce hospital readmissions in patients with heart failure.
- Data and physician note review: There is some controversy surrounding the idea of opening physician notes to patients. Transparency to this extent has never been part of medical practice. Yet, it is being met with some success. Recent research shows that it informed patients and improved patient satisfaction. It also eased physician fears about the idea.
- 99 doctors participated in the OpenNotes exercise and 4,592 patients read at least one doctor’s note. The survey found that among patients:
- 7% of patients contacted their doctor’s office about their note
- Of these, 29% perceived an error
- 85% were satisfied with its resolution
- 37% reported feeling better about their doctor
- 62% reported feeling the same about their doctor
- 7% of patients contacted their doctor’s office about their note
- Doctors were uncertain about the exercise from the outset:
- 26% anticipated documentation errors
- 44% thought patients would disagree with notes
- However, physicians’ opinions changed after a year. The survey found:
- 53% believed patient satisfaction increased
- 51% thought patients trusted them more
- 99 doctors participated in the OpenNotes exercise and 4,592 patients read at least one doctor’s note. The survey found that among patients:
- Pamphlets, printouts, peer groups: The traditional methodologies of patient education still work. For example, according to a report in The American Journal of Medicine, 50% of patients with chronic disease have poor compliance with medication regimens. However, when those patients received educational materials, along with imaging referrals and physician consultations, “67% were compliant with treatment after 6 months.”
Peer groups provide ongoing support for a wide range of conditions and diagnoses. Although clinical data is scant regarding the efficacy of peer groups in improving health and wellness, anecdotal data is widespread. Organizations from Mayo Clinic to the National Kidney Foundation promote peer groups because they can provide emotional and mental support, improve coping skills, and compliance with treatment plans for chronic disease.
The End Goal: Health Literacy
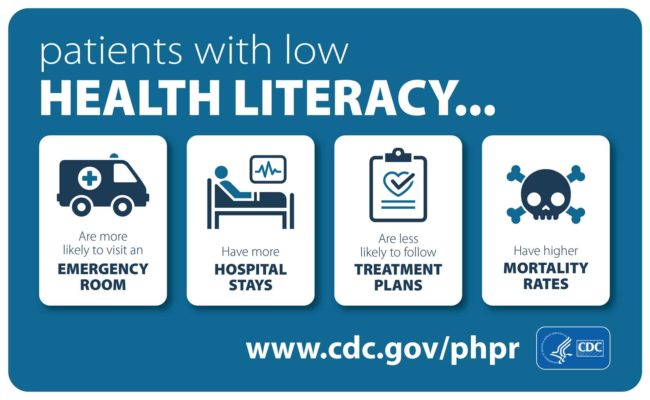
Health literacy is the “capacity to seek, understand, and act on health information”. Patients with high levels of health literacy are able to engage in their own care. They are also able to engage with their providers and get more out of their healthcare experience. They can: :
- Navigate the health system to find the services they need
- Clearly articulate their needs
- Understand healthcare choices and process information
- Decide which treatments are best and act on them
It’s a two-way street. As providers educate their patients, health literacy tends to increase. By the same token, as patients have more experience with the healthcare system, they tend to have higher levels of health literacy. It improves their ability to understand diagnoses, care plans, and the importance of compliance.
The ability to use health technology improves health literacy as well.
- The more that patients use digital health tracking devices and conduct research on the internet, the higher their health literacy. One study suggested that physician ask patients about their eHealth literacy, because of the positive impact it can have on their health.
- Certainly, social media has its pros and cons. However, one study suggests that it can play an important role in educating people about conditions that may still have a stigma attached to them, like mental health issues.
- Wearable fitness devices give patients more information on which to act, and monitor, their own health. When they have more information they can be more engaged in their own health.
- Digital health literacy also helps patients to use patient portals and navigate electronic medical records, when available to them. The more that patients are comfortable with online platforms, the more health information can be pushed to them.
Health education and health literacy are two sides of the same coin. It’s one that pays dividends for the healthcare system at large, providers and patients. Educating patients is no longer an extracurricular event. It has to be part and parcel of the delivery of care. Information increases patient engagement and it can lead to patients improving their own health. That is something that every physician pines for.