The Radiology CORE Exam is the first exam you will take on your road to become a Radiologist testing you on key concepts related to radiology as well as physics. This complex exam can be an exhausting endeavor for test takers. Be ready for the boards by taking sample questions to identify weak spots. See where you stand with these sample Radiology CORE Review Questions from BoardVitals.
Sample Radiology CORE Board Questions
Question 1: Which of the following artifacts is displayed on the ultrasound image?

- A. Side lobe artifact
- B. Mirror image artifact
- C. Speed displacement artifact
- D. Reverberation artifact
- E. Grating lobe artifact
Answer: D. Reverberation artifact
Explanation:
A) Incorrect. Side lobes artifact is created by detection of low-amplitude ultrasound waves, which project radially from the main beam axis. These detected waves will erroneously place objects outside of the field of view onto the image. This is commonly seen as abnormal signal in anechoic structures such as the urinary bladder or gallbladder.
B) Incorrect. Mirror image artifacts occur when the beam encounters a highly reflective interface. Echoes are reflected from the interface back towards the transducer, but then encounter the “back” of a structure, are reflected back to the original reflector and then reflected back to the transducer. This results in a duplicated structure or “mirror image.” This commonly occurs at the diaphragm.
C) Incorrect. Speed displacement artifact occurs when the velocity of sound is decreased below the assumed 1540 m/sec due to an attenuating lesion resulting in a delay of the returning echo. The image processor will erroneously place the tissue posterior to the attenuating lesion deeper than they are truly located.
D) Correct. Reverberation artifact occurs when two parallel highly reflective surfaces repeatedly reflect the beam back and forth before returning to the transducer at different times. These delayed echoes will be shown as multiple linear reflections, which are equidistant from each other.
E) Incorrect. Grating lobes are produced in multielement transducers and result from division of the transducer into smaller elements. These off-axis beams are more perpendicular to the main beam axis compared to side lobes. Grating lobe artifacts are similar to side lobe artifacts, but occur closer to the transducer.
REFERENCES: Feldman MK, Katyal S, Blackwood MS. US artifacts. Radiographics. 2009 Jul-Aug;29(4):1179-89. http://www.ncbi.nlm.nih.gov/pubmed/19605664Kremkau FW. Diagnostic ultrasound principles and instruments. 5th ed. Philadelphia, Pa: Saunders, 1998; 147–157, 377–436 Hangiandreou NJ. B-mode US: basic concepts and new technology. RadioGraphics 2003;23(4): 1019–1033.
Question 2: A 28 year old male had a fall from a 30 foot height. Before being intubated due to hypotension, he reported extreme right sided pelvic pain. Trauma series pelvic radiograph and an axial CT image from a trauma pan-scan are shown. In addition to IV fluids and pelvic stabilization, what would be the next step in management?


- A. ICU monitoring only
- B. Open surgical hematoma evacuation and packing
- C. Embolization of pelvic arteries
- D. CT guided drainage catheter placement
- E. Systematic radiography of both lower extremities
Answer: C. Embolization of pelvic arteries.
Explanation:
As seen on the radiograph performed with the patient on a trauma board, the patient has sustained a vertical shear type pelvic fracture on the right. This is evidenced by the (bilateral) sacral fractures and the craniocaudad translation of the right pubic rami fractures relative to each other. The most common mechanism for this fracture is fall from a height, as was the history in this case. The axial CT image demonstrates extensive extraperitoneal hematoma, both adjacent to the sacrum and extending anteriorly such as anterior to the iliac vessels and iliopsoas muscles. Pelvic bleeding in patients with pelvic fractures may be arterial, venous or through the marrow (“bone bleeding”), with the most concerning obviously being arterial bleeding. In cases of hemodynamic instability, the patient is resuscitated with fluid (and blood), undergoes stabilization of the pelvic fractures (such as with external fixation) and undergoes angiography to embolize arterial bleeding. Whether to perform orthopedic stabilization or angiography first is variable, with some maintaining that orthopedic hardware may obscure angiographic imaging so angiography should be performed first. Open surgery for extraperitoneal bleeding is only done in patients who remain persistently unstable. CT guided catheter placement is not performed as the presence of hematoma partially tamponades potential additional bleeding. Radiography of the lower extremity is indicated in patients with falls from heights who commonly sustain other fractures such as pilon fractures, talar fractures and calcaneal compression fractures; however, in hemodynamically unstable patients, hemodynamic stability must be accomplished first.
References: 1. Geeraerts T, Chhor V, Cheisson G, Martin L, Bessoud B, Ozanne A, Duranteau J. Clinical review: initial management of blunt pelvic trauma patients with haemodynamic instability. Crit Care. 2007;11(1):204. 2. Uyeda J, Anderson SW, Kertesz J, Rhea JT, Soto JA. Pelvic CT angiography in blunt trauma: imaging findings and protocol considerations. Abdom Imaging. 2010 Jun;35(3):280-6.
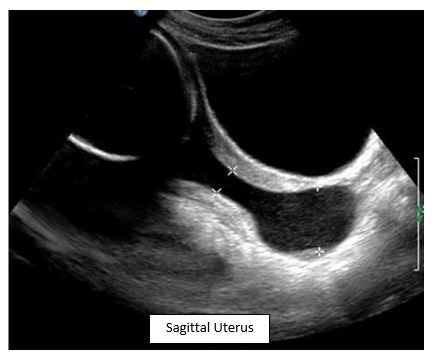
Question 3: What is most commonly associated with this finding during a second trimester ultrasound?
- A: Polyhydramnios
- B: Fetal anomalies
- C: Intrauterine growth restriction
- D: Preterm delivery
Answer: D. Preterm Delivery
Explanation:
This is an example of cervical funneling in cervical incompetence. Most cases are idiopathic, but known causes include previous preterm delivery, previous cervical procedures and DES exposure.
Incorrect Answers:
A. Oligohydramnios is associated with cervical incompetence from premature rupture of membranes.
B. and C. This is not associated with cervical incompetence.
Looking for additional practice before test day? The BoardVitals Radiology CORE Review Question Bank contains over 1,300 Questions targeted to the ABR CORE Exam blueprint. Sign up for a free trial today!




